When Peripheral Artery Disease (PAD) Affects Quality of Life
September 22, 2024Walking shouldn’t be painful — and in most cases, it’s not just a normal sign of aging. Yet, far too often, patients who experience claudication — the clinical term for leg pain that occurs during activity, such as walking — simply ignore the pain or mistake it for another problem. However, pain in the legs that occurs while walking is the most common sign of peripheral artery disease (also known as PAD). Patients with PAD in its early stages experience pain while they’re moving, but the pain goes away with rest. It’s easy to see how this common symptom can have a real impact on quality of life. Everything from walking, grocery shopping, traveling, or playing with grandchildren is harder when it hurts. This article explores everything you need to know about PAD, with insight from WakeMed’s medical director of Vascular Surgery Dr. Ellen Dillavou.
What is PAD?
Peripheral artery disease is the often underdiagnosed and undertreated ‘cousin’ of heart disease. It’s a common circulatory problem that occurs when the arteries become narrowed or blocked due to plaque buildup (atherosclerosis). This in turn reduces blood flow to the limbs, which can cause pain or discomfort. When organs and tissues don’t get the blood flow they need, they can become damaged over time — leading to tissue damage or death (gangrene). Gangrene from PAD typically occurs in the toes and/or feet and can result in amputation.
PAD Signs, Symptoms and Risk Factors
While most of us are aware of heart disease, its risk factors and complications, PAD gets a lot less attention — and often goes undetected. Because both PAD and heart disease are caused by plaque build-up, they’re often linked — making early diagnosis and treatment important to prevent further complications, such as heart attack or stroke.
Signs & Symptoms
- In some cases, PAD can be mild or have no symptoms.
- Pain, discomfort, fatigue or cramping in the calf or hip muscles when walking or climbing stairs that goes away with rest
- Numbness or weakness in the leg(s)
- Coldness in lower leg or foot, when compared to the leg/foot on the other side of the body
- Sores or wounds on toes, feet or legs that have difficulty healing
- Change of color or shiny skin on the legs
- Hair loss or slower hair growth on feet/legs
- Slowed growth of toenails
- Zero or weak pulse in legs or feet
- Erectile dysfunction in men
- Aching or cramping in the arms when performing manual tasks
Am I at Risk for PAD?
Risk factors for peripheral artery disease include:
- Smoking or tobacco use (80% of patients with PAD are smokers or former smokers)
- Having Type 2 diabetes
- Being over age 50 (risk increases with age)
- Having a personal or family history of heart or blood vessel disease
- Having high blood pressure and/or high cholesterol
- Having a blood clotting disorder
- Having kidney disease or being on dialysis
Diagnosing PAD
Patients who think they may have PAD should talk to their primary care doctor or cardiologist. In most cases, the physician will begin with a visual exam, looking carefully at your feet and legs for signs of disease. They’ll also talk to you about your medical history, risk factors and any signs or symptoms you may have. Additional testing may include an ultrasound test called an ankle/brachial index (ABI), which will measure the blood pressure in both your legs and arms to compare and evaluate blood flow
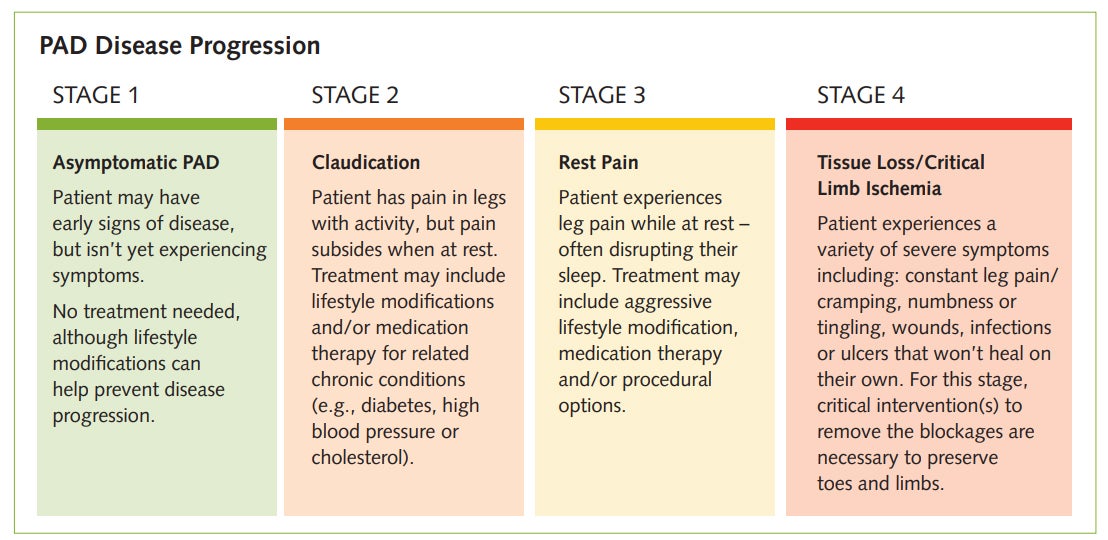
in both areas. Angiography can locate the specific areas of blockage. Yet, because PAD is so prevalent, it’s often present without symptoms. But Dr. Dillavou explains that treating PAD is really only necessary for those patients whose disease is affecting their quality of life.
“Because all treatments come with inherent risks, we don’t typically treat asymptomatic patients,” explains Dr. Dillavou. “Instead, we’ll start with basic lifestyle modifications and move onto treatment only when and if symptoms arise. The goal of treatment for PAD is truly to improve quality of life and to ensure we preserve all toes and limbs for the long-term.”
WakeMed Resources for Patients With PAD
WakeMed Vascular Surgery
Our team of experienced vascular surgeons offer the most advanced care for patients with PAD, including diagnosis, disease management and the latest minimally-invasive endovascular procedures.
Offices in Cary, Raleigh and Midtown Raleigh 919-350-7600
WakeMed Wound Care
Many patients with PAD experience non-healing wounds that, if left untreated, could lead to toe or
limb loss. WakeMed Wound Care offers diagnostic testing, nutritional evaluation, pressure-relieving
devices and specialized dressings, infection control, education and hyperbaric oxygen therapy.
Offices in Cary and Raleigh 919-350-4515
Quit With WakeMed
Our virtual tobacco cessation program can help patients reduce or quit the use of tobacco, following a proven model that is approximately 10 times more effective than quitting on your own. Treatment options may include medication, counseling or a combination of both, and you’ll meet with your tobacco treatment team regularly so you can stay on track.
Virtual Tobacco Cessation Program 919-350-QUIT (7848)
Heart to Heart Magazine
Heart to Heart is published quarterly for patients, former patients and physicians associated with the WakeMed Heart Center. Discover heart-healthy recipes, the scoop on the latest trends in nutrition and the extraordinary men and women who work within the Heart Center’s walls.
Read the latest edition and subscribe today.
