Apex Emergency Department Teams Up with Telestroke for Brain-Saving Care: Marcia Gave's Story
October 1, 2024
July 20, 2024, was a typical Saturday with lots of chores. Around 8:10 am, Marcia Gave was doing laundry when suddenly she realized she was on the floor with no awareness as to how or why this happened.
Her husband, Byron, was in a nearby room when he heard unusual sounds, including the rustling of clothing and the swooshing of a plastic bag.
"I wondered why I was hearing this, so I peered around the corner to find my wife sitting on the floor in the laundry room."
Byron could see her face was turned downward on the right side, she had a blank expression and was unaware of her environment. Byron also observed that her right arm and leg were in a crooked position. He knew immediately that something was terribly wrong.
"I asked her if she fell," shares Byron. "She wasn't able to respond."
Marcia recalls, "I don't remember him asking me anything. I only remember my husband trying to put my shoes on, my efforts to help him and my realization that I could not."
Byron, feeling helpless, sat for a moment on the floor holding his wife, tears rolling down his face, yet he assured her that everything would be okay. He then lifted her up, helped her steady herself on her functioning left leg and walked her across the room to a nearby chair.
"I told her to sit and wait for me while I went to retrieve an outfit to change her into since she was wearing pajamas. I didn't know where exactly to go, but I knew I was taking her to an emergency room."
A Swift Ride to WakeMed Apex Healthplex Emergency Department
Byron maneuvered his wife into the vehicle around 8:30 am and asked Google for the nearest emergency department. Google Maps then navigated the couple to WakeMed Apex Healthplex Emergency Department where they arrived around 8:45 am. Marcia's stroke symptoms had been going on for 35 minutes by that time.
Marcia remembers, "He asked me if I could hook my seatbelt. I looked at it, and I just couldn't. I could have used my left hand, but I didn't even know how to do it in that moment. I had no emotion during this time. It was like that part of my brain turned off, which is odd since I am a worrier."
Byron pulled up to the emergency entrance and helped Marcia hobble on her left leg, while he supported her paralyzed right side. He then placed her in the hospital entry wheelchair and whisked her to the front check-in desk.
"It was absolutely amazing," recalls Byron of the reception he received from the care team. "It was like they were waiting for us. It felt like divine intervention that brought us to this emergency department."
An Expert Care Team Gets to Work
The care team took Marcia to the back and immediately stepped into action with swift care.
Marcia shares, "They were doing all this stuff, and I was lying down surrounded by a lot of people. I was being hooked up to monitors with intravenous (IVs) in my right arm. Yet, I only remember thinking how pretty the technician was, and I wanted to tell her, but I couldn't talk. It was bizarre."
Adam Rutz, MD, an emergency department physician, ordered a computed tomography (CT) scan of her brain and a computed tomography angiography (CTA) and received Tenecteplase within 25 minutes of arrival. Marcia also underwent magnetic resonance imaging (MRI) and was diagnosed with an ischemic stroke.
"Dr. Rutz was absolutely so self-assured," says Byron. "He knew exactly what to do. He asked a member of the care team to set up a telestroke visit with neurologist Melanie Winningham, MD, located in Virginia.
The Winning work of the Telestroke Team
Byron watched in awe as they discussed the symptoms, treatment options and administration of Tenecteplace for her stroke symptoms. After Byron gave consent for treatment and administration began, he saw his wife slowly come back.
"It was absolutely astonishing how unbelievably, incredibly capable they were and how they were so quick to decide exactly what to do and how to do it," offers Byron.
Dr. Winningham had Marcia perform a variety of movements and had her answer questions using a standardized stroke test.
Marcia says, "I could see everything that was going on, but I couldn't speak. I remember shaking my head to respond and them asking me to try to speak, but gibberish came out. Dr. Rutz was close to my face to keep me focused. I was thinking, 'I have to pay attention, and I have to answer the questions.' They showed me the picture three or four times, within minutes apart and with each encounter, I was able to say a little bit more. Then suddenly, I looked at my husband and said, 'Today is our granddaughter's birthday party, and we're gonna miss it."
Byron observes, "It happened so quickly. She went from being unable to talk with a drooped face to talking and her face slowly returning to normal."
A Transfer to WakeMed Cary Hospital, a Joint Commission-Certified Primary Stroke Center
Dr. Rutz had WakeMed Mobile Critical Care transfer Marcia to WakeMed Cary Hospital, around 10:15 that morning, for admission to the Intensive Care Unit to closely monitor her.
Dr. Rutz reflects on the experience. “It was an all-hands-on-deck, team effort to get Mrs. Gave the care she needed. After her initial assessment, it was clear Mrs. Gave had serious and significant symptoms of a stroke, and with telestroke consultation, we offered her tenectaplase, a thrombolytic, or “blood clot dissolving” medication.”
Once settled into the intensive care unit (ICU), the couple contacted their son to explain that they would not make it to their granddaughter's party but not to worry because Marcia was stable and would make a full recovery.
While in the ICU, the care team came to their room every 15 minutes and asked Marcia to share her name, what happened, where she was and to perform a series of facial expressions, including smiling, raising her eyebrows, touching her nose, moving her arms and legs and answering additional questions.
With a successful overnight stay, Marcia was then transferred to a step-down unit and sent for a transesophageal echocardiogram (TEE). The team needed to determine if she had any heart issues that could have caused her stroke. She was diagnosed with a patent foramen ovale (PFO), a condition in which a small opening remains between the heart's two upper chambers after birth. With this confirmed, they knew they would need further testing of Marcia's heart. Stephen Boateng, MD, a WakeMed cardiologist, ordered a wearable heart monitor, so he could determine if the PFO or another heart condition caused the stroke.
"Dr. Boateng and everyone were fabulous. My nurse, Grace, was amazing and encouraging and one of the best nurses from whom I've ever received care," notes Marcia.
Byron adds, "We recently moved to this area on May 22 and left a good health care system. WakeMed is superior. We are amazed by the quality of care, efficiency and capability of these professionals in every single encounter."
Discharge Home with No Side-Effects of Stroke
Marcia was discharged home, in the care of her husband on July 22. Anna G. completed the transition of care and before discharge the physical therapy team thoroughly tested Marcia's abilities asking her to repeat phrases, demonstrate her ability to walk and stretch as well as show strength in her arms and legs. Marcia passed the test and was scheduled for follow-up with her primary care doctor and in September with Dr. Boateng.
Marcia glows, "I was so excited to get out of the hospital. The next day was my granddaughter's actual birthday, and we got to see her."
Marcia also visited an orthopaedic specialist to ensure she hadn't fractured any bones during her fall in the laundry room. She was cleared with no broken bones.
On September 3, Marcia and Byron visited Dr. Boateng to determine if heart issues were the root cause of the stroke.

The heart monitor observation proved that atrial fibrillation (AFib) was not present. Dr. Boateng concluded it would be worth seeing a structural cardiologist for advice on whether or not to close the PFO hole.
Dr. Boateng observes, "Once it was established by the neurologist the stroke was most likely a clot that came from her heart and embolized in her brain, we had to move determine if she had an abnormal rhythm caused by atrial fibrillation or an atrial flutter. We had her wear a monitor. I also did the TEE to view her heart, where I found the PFO. After the heart monitor determined she did not have an abnormal rhythm, we determined the most likely cause of her stroke was a clot that began in her leg, and traveled to the right side of her heart. Because of the PFO, it had access to travel to the left side of her heart and was pumped into her brain. PFO closure would prevent that from happening again."
Andrew Sampson, MD, a WakeMed interventional cardiologist, agreed that the hole should be closed. With additional confirmation at Marcia's appointment on September 25 with her neurologist, she is scheduled for the repair on October 16.
Dr. Sampson explains, "PFO closure is indicated for those patients who have suffered a stroke that is felt to be due to the passage of a small clot through the PFO. Typically, this is a diagnosis of exclusion as approximately 25 percent of the population has a PFO, and the vast majority never have an issue related to it. Closure of PFO for this select population can result in a significant reduction in the risk of a second stroke."
Marcia's Life Today
Marcia has returned to her normal, leisurely retired life with her husband. She now wears a smartwatch, so in the event of an emergency, a medical alert will be issued. Byron is now hypervigilant about his wife's care, mostly sticking by his wife's side.

"Byron and I love spending lots of time with our family here in Cary, which includes a fabulous granddaughter and a fabulous grandson! We also take walks and go to our clubhouse gym. We have at least one lunch or dinner date every week, listen to several music genres and spend far too much time on Netflix! We just got back from visiting our Michigan son and his wife and the rest of our family and friends that we miss so much."
About WakeMed Stroke Program
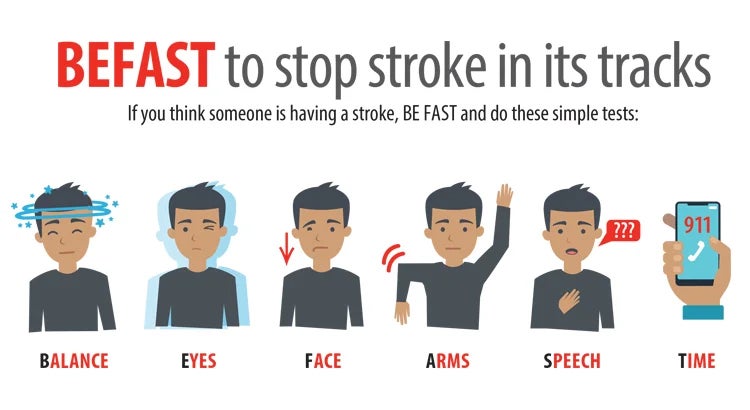
Each year, thousands of families in our community are impacted by stroke — it can occur at any age.
At WakeMed, we offer a full continuum of compassionate, innovative stroke care — from diagnosis in our emergency departments to rehabilitation in both our award-winning inpatient and outpatient facilities.
As leaders in stroke care, we also collaborate with hospitals through our Telestroke Program. Our Telestroke Program neurologists evaluate patients experiencing sudden onset of stroke symptoms in our WakeMed emergency facilities.
WakeMed's Award-Winning Stroke Program
WakeMed Raleigh Campus and Cary Hospital are Joint Commission Thrombectomy Capable Stroke Center and Joint Commission-Certified Primary Stroke Center that also performs Thrombectomies. We’ve also received the Joint Commission Gold Seal of Approval for Stroke Care.
Our Stroke Program is distinct in providing a comprehensive approach, moving from prevention to management. Our dedicated team of specialists, renowned for their expertise, use physical medicine and rehabilitative techniques at strategic steps along the route to recovery to support the best outcomes. Here are just a few of our impressive features:
- Collaboration with EMS providers to facilitate rapid assessment and transport to the hospital
- Team approach that helps minimize time from arrival to administration of thrombolytics
- Availability of neuroradiologists for quick, expert interpretation of imaging
- Neurology and neurosurgery coverage 24 hours a day, seven days a week for evaluation and treatment
- Neuro intensive care unit for optimization of care for patients with severe strokes
- Nursing staff skilled in assessment and care of stroke patients
- Designated nursing unit for the care of patients with neurological and neurosurgical diagnoses
- Interdisciplinary care planning involving physicians, nurses, case managers, therapists and other services such as nutritionist consultation and pastoral care
- Comprehensive post-discharge rehabilitation services, including specialty services, such as vestibular rehab to treat dizziness and vertigo and stroke VNS rehab to improve upper limb function for stroke survivors
- Public education and awareness programs that focus on risk factor reduction for stroke prevention
- A variety of stroke support groups at several locations throughout North Carolina
WakeMed has also been awarded top honors from the American Heart Association and American Stroke Association for success in implementing a higher standard of care for stroke patients. We are accredited by the Commission of Accreditation on Rehabilitation Facilities (CARF), due to our comprehensive inpatient rehabilitation programs and commitment to specialty rehab. Our Stroke Program is Stroke Specialty Program Certified (CARF-SSP).
Additionally, WakeMed Raleigh Campus has received official certification as a Thrombectomy-Capable Stroke Center from The Joint Commission. This certification is the second highest of the four advanced stroke certifications offered by The Joint Commission in collaboration with the American Heart Association/American Stroke Association. This certification recognizes hospitals that meet rigorous standards for performing endovascular thrombectomy and providing post-procedural care for patients.
About WakeMed Heart & Vascular
WakeMed Heart & Vascular physicians bring together expert cardiovascular, thoracic and vascular surgeons who are dedicated to delivering the highest level of cardiovascular care in Raleigh, Apex, Cary, Fuquay-Varina, Garner and Clayton, N.C. For decades, these physicians have chosen to bring their talent and expertise to WakeMed for its reputation for excellence in cardiovascular care and commitment to providing the most exceptional patient experience.