Dr. Amantia Kennedy on the Magic of Menopause
August 12, 2024
By: WakeMed Health & Hospitals
Categories: Women's
Tags: May is Women's Health Month, women's health month, Women's Health, Menopause, Perimenopause
Incredible.
Beautiful.
Magnificent woman.
From puberty to the menopausal transition, a woman's body is a wonder.
Womanhood is more than fertility and youth.
All stages of female development are amazing — the metamorphosis from childbearing to graceful aging is no different.
Let's take a deep dive with Amantia Kennedy, MD, FACOG, of WakeMed Obstetrics & Gynecology, into the menopausal transition and what women can expect as their bodies release the final eggs and move into a new, glorious stage of freedom in womanhood.
Is it just a women's thing?
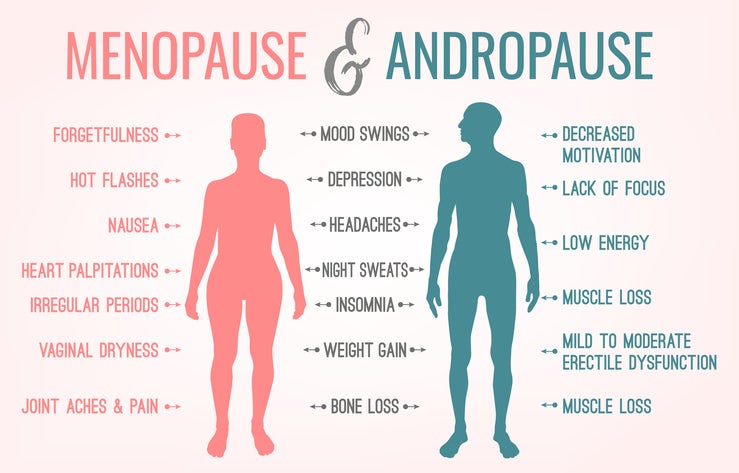
First, it's interesting to note that hormonal transitions in fertility apply to both men and women. While women go through menopause, men undergo andropause. Aging happens in all sexes, so women should feel confident that this is normal, anticipating the changes with intrigue and hope.
What exactly is menopause?
Menopause is the final period in a woman's reproductive life. It is diagnosed after twelve consecutive months of amenorrhea (absent periods) due to the lack of hormonal production from the ovaries. The timing of menopause is based on a woman's age and other risk factors.
Why does menopause happen?
Women are designed this way, so it’s important and even comforting to understand that they are not alone and their experiences are not an anomaly. Women are born with a certain number of eggs, around 400,000. Women start to recruit these eggs in adolescence during puberty. Each menstrual cycle, the body selects a number of those eggs as candidates for ovulation, ultimately choosing one as the dominant egg to release while the rest of the candidates for that cycle are reabsorbed by the body. So, each month starting at puberty, women recruit these eggs during the reproductive years until they run out, which is the onset of menopause. Women's bodies continue to produce hormones but not to the degree of that in the reproductive years.
Menopause, which ends the production of ovulatory eggs, happens at different times for different women. The length of the transition into menopause varies from woman to woman. Some women will enter the transition in their early forties, some mid-forties and some late forties.
That transition into the menopause (perimenopause) is characterized by irregular cycles. Cycles may come a bit later than normal. Some women will skip a month. Once this starts, a woman will predictably achieve menopause within one to three years.
During perimenopause, a lot of hormonal changes and fluctuations happen. Modern medicine allows doctors to understand that women will start to have some of these experiences years before the complete end of monthly cycles.
What are some common symptoms of menopause?
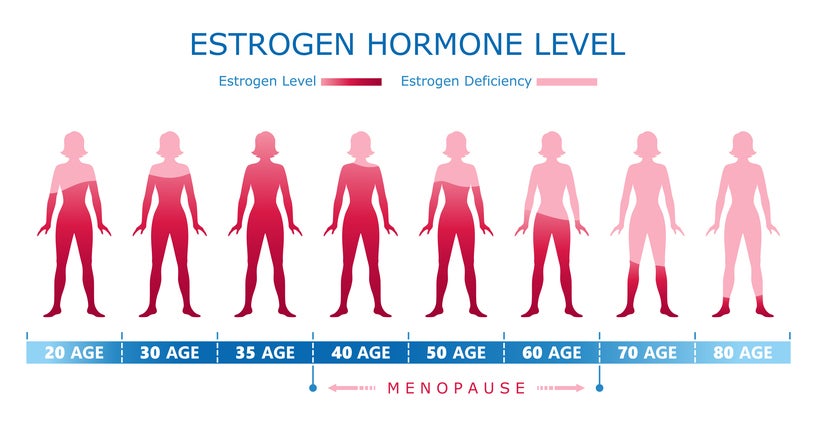
Estrogen is produced in the ovaries, and as the main female sex hormone, it is needed for puberty, the menstrual cycle, pregnancy, bone strength and other functions. Estrogen levels vary throughout the menstrual cycle and fall after menopause. When production decreases, organs throughout the body are affected.
Here are some results:
- Hot flashes, also called vasomotor symptoms, are the most common symptom of menopause. Hot flashes cause a sudden feeling of warmth, usually most intense on the face, neck and chest. A woman's skin may redden, and she may experience profuse sweating.
- Night sweats can also appear during this time. They are essentially hot flashes at night, during sleep.
- Lost muscle mass and weight gain happen naturally with aging. During the menopausal transition, muscle loss is accelerated due to the low estrogen levels. This results in more pronounced weight gain, most concerningly, the visceral fat around internal organs.
- Visceral fat around the organs causes inflammation in the body, which in turn leads to an increase of insulin resistance, which in turn leads to greater occurrences of type two diabetes, cardiovascular disease, etc.
- Brain fog happens because estrogen increases blood flow to the brain, and when those estrogen levels drop, the brain has to acclimate. In addition to the effects on blood flow in the brain, estrogen enhances brain metabolism, improves brain connectivity, boosts activity of serotonin and clears some amyloid deposits, which are the proteins that contribute to Alzheimer's disease. So, when this change in hormonal fluctuation occurs during perimenopause and finally menopause, it affects the brain, and women, in turn, complain of feeling off and forgetful.
- Forgetfulness is common. Women will state, "I forgot a meeting. I can't find my keys," etc. The good news is that findings show menopause does not impact a woman's cognitive ability or ability to process information. It instead impacts the ability to take in new information. The good news is that it is temporary.
- Sleep disturbances, including difficulties falling and staying asleep, occur during menopause due to the fluctuation of the hormones.
- Depression and anxiety can also be associated with this transition.
- Elevated heart rate is common and could include heart palpitations and heart racing.
Does menopause cause changes in a woman's vagina?
Hormonal fluctuations cause changes in the vaginal discharge that women experience from month to month. During perimenopause, the hormonal functions are unpredictable, so a woman may be caught off guard by the discharge since it can come and go and change out of rhythm with her cycle. Vaginal itching, vaginal discomfort, vaginal dryness, changes in vaginal acidity and changes in vaginal odor are common.
Also worth noting, changes in the elasticity of collagen in the vagina means the vagina can shrink a little and become thinner, making the friction from intercourse sometimes painful.
A decrease of blood flow to the vaginal mucosa, vaginal tissue and to the vestibule, leads to changes in the clitoris. Those changes to the clitoral hood include some shrinkage. Similar to what a woman is experiencing, a man's penis shrinks a little with age as well.
What help is available to treat menopausal symptoms?
Hormonal and non-hormonal remedies are available. Hormone therapy may include estrogen and progesterone for women who have a uterus or estrogen, alone, may be administered to women who do not have a uterus.
Non-hormonal therapies include newer medications on the market, specifically targeting the part of the brain that regulates the internal bodily thermostat. It can effectively reduce hot flashes and nights sweats by 80 percent. Other non-hormonal medical treatments for women who either don't want the hormones or have contraindications to hormones are in the antidepressant family.
An anti-epileptic medications is very effective in low doses for management of night sweats and sleep disturbances. Antihypertensive medication is another option.
The bottom line is that there is help, and women should discuss their symptoms with their medical providers.
What about natural remedies for hot flashes?
The most effective natural remedy for hot flashes is cognitive behavioral therapy since it supports the mind and body connection. It's the mind telling the body that this is temporary. Normalizing it helps to eradicate fear as it supports acceptance that this a short-lived season in life.
Women should also talk about lifestyle modifications with their medical providers.
What can a woman do to improve her sex life during menopause?
A woman can improve her sex life in a variety of ways.
- If she simply has vaginal dryness, a water- or silicone-based lubricant can be used to make intimacy more comfortable.
- Vaginal moisturizers with hyaluronic acid are also effective. Women can also improve with medical treatment.
- Hormone therapy with estrogen can help and has minimal side effects without progesterone included. It helps with elasticity and lubrication of the vagina.
- Vaginal steroid suppositories are another option. They convert locally to testosterone and estrogen in the tissues of the vagina.
How does a woman address accompanying menopausal depression and/or anxiety?
A psychiatrist, family practitioner and gynecologist are very in tune with what's happening during this time. It is important to first and foremost talk with a doctor who has a special interest in menopause.
The signs of depression and anxiety can be accelerated during menopause. During the menopausal transition up to 37 percent report experiencing anxiety and as many as half report depression.
This happens because some women have a reduced ability to adapt to the hormonal changes as a result of other risk factors. These could include the following:
- Childhood trauma is associated with an increased risk for depression during the menopausal transition.
- Socioeconomics structures, such as financial difficulties can have a bearing.
- Ongoing care responsibilities to partners, children and parents during the transition can increase risks.
Do women need less sleep during menopause since they may struggle with sleep?
The need for seven to eight hours of sleep a night does not change with menopause. Sleep disturbances, such as sleep apnea, insomnia, hot flashes, depression and more make sleep very difficult during this time, so treatment is critical.
Women should talk to their provider about their condition and any medications or supplements they may be taking that are contraindicative to sound sleep.
Sleep hygiene is also especially important during the menopausal transition. Women should sleep in a quiet, cool, dark environment. They should avoid screen time at least an hour before bed. They should also avoid exercising close to bedtime.
How can a woman maintain bone health during menopause?
Estrogen is a major player in bone formation. Major bone loss occurs during this period and continues for years after. Yet, bone loss begins in our thirties.
Young women and women throughout the life span should take the following actions:
- Start supplementation.
- Refrain from smoking or start smoking cessation.
- Eat a healthy diet, rich in calcium and vitamin D.
- Participate in strength training.
- Avoid alcohol because more than 6 ounces of wine per day is associated with an increased risk for low bone density.
Early menopause is another risk factor for bone fragility. Women who go into menopause under the age of 45 should take extra care since they will have more years (in a typical lifespan) for which bone density will be decreasing.
Additionally, even with all these precautions, genetics can be a risk factor, so it's important to obtain a thorough history of parents and sisters and the impact of certain medications, including steroids.
Aromatase Inhibitors for patients with breast cancer, heavy use of marijuana, autoimmune conditions, rheumatoid arthritis and Type 2 diabetes are all associated with an increased risk for bone loss.
Medical treatments are available specifically for bone loss. Among those, hormone replacement therapy is very effective.
Does menopause make a woman less of a woman?
Women are more than baby makers, just as men are more than sperm donors. Menopause does not detract from a woman's value and purpose. It is FREEDOM from monthly period cycles, contraception and the risk of becoming pregnant — which can positively impact intimacy.
Women should take pride in aging and take precautions to age well, including being screened for diabetes and cardiovascular disease.
About Amantia Kennedy, MD, FACOG
 Dr. Amantia Kennedy is an obstetrician/gynecologist with WakeMed Physician Practices - Women's Center. Her clinical interests include infertility, menopause, high-risk obstetrics as well as minimally invasive and robotic-assisted surgery.
Dr. Amantia Kennedy is an obstetrician/gynecologist with WakeMed Physician Practices - Women's Center. Her clinical interests include infertility, menopause, high-risk obstetrics as well as minimally invasive and robotic-assisted surgery.
Dr. Kennedy earned her medical degree from the Texas Tech Health Sciences Center School of Medicine-Lubbock Campus and completed her residency in the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill. She also has a Bachelor of Science degree from Lubbock Christian University in Lubbock, TX. As a resident, she won numerous awards, including “Best Teacher of the Year” and “Special Resident of the Year.”
She is a member of the American College of Obstetricians and Gynecologists and the American Medical Association and is a Pyramid Society Award recipient.