Fall Prevention Tips That Save Lives
September 23, 2024
By: WakeMed Health & Hospitals
Categories: Primary Care, Urgent Care, Emergency
Tags: fall prevention, injury prevention, aging in place, fragility
Medically reviewed by Ann Pearce, PT, DPT
September 23 to 27, 2024, is Falls Prevention Awareness Week.
Falling doesn't have to be an inevitable aspect of aging. Falls can be prevented by proactively fall-proofing the home, discussing risk factors, remaining physically active and more.
Staying Safe at Home
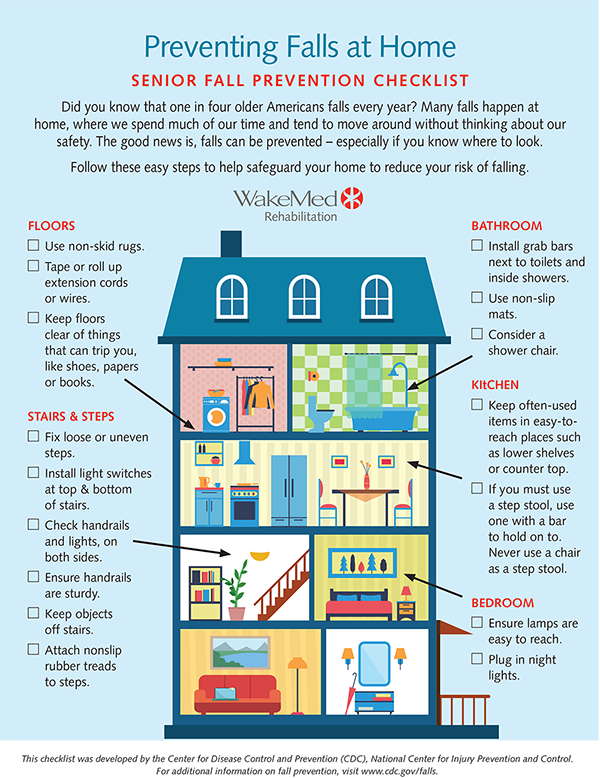
Home safety is always a big deal, but it becomes especially important to prevent slips, trips and falls — as people age or experience a decline in physical dexterity. A comprehensive approach to falls prevention begins with a thorough assessment of the living environment, identifying potential hazards.
One of the most critical areas to address is flooring. From non-slip surfaces to removal of electrical cords, much can be done to prevent injury. Additionally, installing grab bars in bathrooms, securing stair railings and ensuring that lighting is adequate in all areas of the home are vital steps that can enhance safety. Incorporating assistive devices — such as, walkers or canes — into daily life can provide extra support when moving about the home as well.
Having Crucial Conversations
Talking with family, friends and health care providers is the best way to improve safety. Open dialogue with older family members about their needs and concerns can often provide valuable insights into what modifications might enhance their comfort and confidence at home. Proactive measures not only help prevent falls but also promote a sense of independence and well-being, allowing them to navigate their surroundings safely and with greater ease as they continue to enjoy their lives. A team approach helps older adults stay active, healthy and able to do the things they enjoy.
Take a look at this step-by-step informational graphic to help determine hazards at home and ways to prevent the risk of falling.
Aging Gracefully in a Strong Body
Exercise is an important part of improving safety, increasing strength and balance. A health care provider can provide a referral to physical therapy for exercises individualized to each patient.
The National Council on Aging recommends community exercise programs to decrease the risk of falling. See more information about Evidence-Based Falls Prevention for Older Adults (ncoa.org).
Search for exercise classes offered in the community on Standing Strong NC.
There are also simple exercises to do at home. It's important to take it slowly and ensure steadiness when engaging in them:
- Sit to stand: Sit in a sturdy chair. Practice standing up and sitting down 10 times in a row.
- Heel raises: Hold onto the kitchen counter with both hands. Rise up on your toes and slowly lower 10 times.
- Side leg kicks: Hold onto the kitchen counter with both hands. Slowly kick one leg to the side. Repeat on each side 10 times.
Ensuring the Rubber Meets the Road
A good pair of shoes should bend, bounce, grip, lie flat and fit.
Rubber shoes are great. Super sticky waffle grip running shoes can be too gummy, and cause tripping.
Loose shoes are out. Shoes should enclose the heel and fit firmly around the feet to hold them in place.
High heels should mostly be a thing of the past, except a block heel for a rare special occasion.
See more comprehensive tips below.

Understanding the Role of Sight and Sound
It's important to have eyesight and hearing tested each year to help prevent falls.
Vision changes are common as people get older and affect balance in many ways. If someone is unsteady when walking, eyesight might be part of the problem.
Depth perception is an important part of vision that can affect safety. For example, if a curb or edge of a stair is hard to see, a person might lose his/her balance and fall.
Vision also serves as a reference point for spatial awareness. If a person's vision is blurry, this can affect the sensory system and lead to falls.
Hearing can also increase falls risk. When people are hard of hearing, they may stop going out with family or friends because it can be embarrassing or difficult to join conversations. They may not enjoy time at restaurants or other busy places simply because they cannot hear.
Less activity leads to reduced strength and balance, increasing the risk for falls.
Poor hearing can also increase the chance of developing mental health conditions, such as depression. Depression is often accompanied by less activity. The domino effect of lost strength and balance from inactivity increases the risk for a fall.
Dealing with a Dose of the Dizzies
Dizziness increases the risk for a fall and is one of the most common reasons older people see a health care provider.
Benign paroxysmal positional vertigo (BPPV), also known as positional vertigo, is typically the reason for dizziness. It is caused by the inner ear and can improve through treatment with a vestibular physical therapist.
While high blood pressure is common with aging, some people develop low blood pressure as they get older. Dizziness can be a symptom of low blood pressure and can worsen when someone gets up quickly, causing a sudden drop in blood pressure. This can lead to falling or passing out. Older adults can also experience low blood pressure if their blood pressure medication dosage needs to be adjusted or they become dehydrated (more common with age).
A visit to a medical provider is important to determine the reason for dizziness. WakeMed Vestibular Rehabilitation can help with dizziness.
Managing Meds
Medications have a complex relationship with the falls risks. Patients should discuss side-effects, dosages and medication interactions with their health care provider.
Three types of medications increase falls risk:
- Sleep aids or medications that have drowsiness as a side-effect can lead to falling. Here are examples:
- Nitrazepam, Diazepam, Temazepam
- Amitriptyline, Dosulepin, Chlorpromazine, Chlorpheniramine
- Phenobarbital, Hydroxyzine
- Muscle relaxants and pain relievers (opioids) can increase the risk of falling. They can cause drowsiness and confusion, which can lead to challenges with walking.
- Anti-anxiety medications (psychotropics) can lead to drowsiness, impaired coordination and slowed reaction times, thereby raising the risk of falls. These medications include:
- Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) like Escitalopram (Lexapro), Sertraline (Zoloft), and Citalopram (Celexa)
- Antipsychotics, which may result in confusion and dizziness
Considering Additional Tips
Ultimately, treating the body well can help prevent falls.
- Get enough sleep.
- Avoid alcohol.
- Stand up and sit up slowly.
Learn more about WakeMed's Balance and Falls Prevention Plan.
About Ann Pearce, PT, DPT
 Ann is a physical therapist who has a special interest in treating patients with vestibular issues (balance, dizziness, etc.) resulting from postural orthostatic tachycardia syndrome (POTS), stroke, concussion, Parkinson’s disease and other issues. She also enjoys helping patients prevent falls. She earned her Bachelor of Arts degree in psychology at Wake Forest University and completed her doctorate degree at Northwestern University.
Ann is a physical therapist who has a special interest in treating patients with vestibular issues (balance, dizziness, etc.) resulting from postural orthostatic tachycardia syndrome (POTS), stroke, concussion, Parkinson’s disease and other issues. She also enjoys helping patients prevent falls. She earned her Bachelor of Arts degree in psychology at Wake Forest University and completed her doctorate degree at Northwestern University.
Ann chose physical therapy as her career path because she wanted to work in a health care profession in which she could spend a lot of time with patients, getting to know them and making a difference in their lives. She loves working with patients with dizziness because she is intrigued with the challenge of finding the root cause of their dizziness and helping them feel better. She also enjoys helping patients build better balance and getting and staying active to prevent falls. In her spare time, she enjoys hiking, reading, cooking and spending time with family.