"My Daughter Recognized My Stroke Symptoms. It Saved My Life."
August 1, 2024
By: WakeMed Health & Hospitals
Categories: Emergency, Stories, Raleigh Campus, Cary Hospital
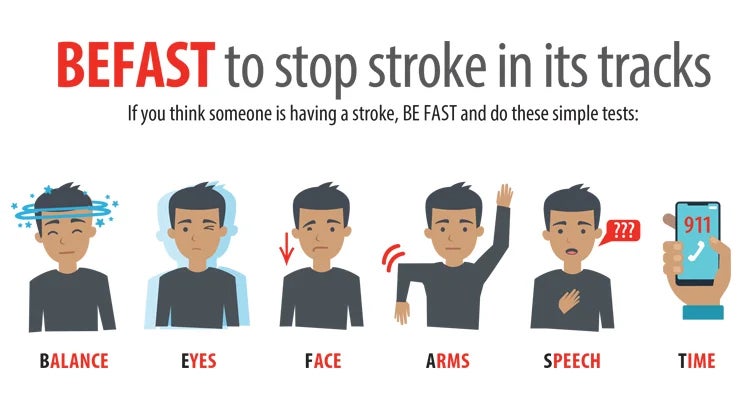
Tags: Brain and Spine, Ischemic Stroke, Stroke Symptoms, BEFAST, Stroke Support Group
Holly Springs residents, Grant Jacobs and his wife, welcomed their daughter and her fiancé who were in town visiting during the Memorial holiday weekend.

"I'd only met my daughter's fiancé briefly once before. They came, so we could get to know each other. We decided to take a stroll that Sunday morning, May 26, 2024. It was fairly hot and humid outside."
Speech Gone Wrong
While on that walk, Grant was mid-sentence sharing a funny story about the family dog, when the words Grant's brain were forming did not match the garbled noise that came from his mouth. He attempted to repeat the phrase realizing that the intonation was not at all correct.
"I sounded like I had a speech impediment or peanut butter stuck in my mouth. My brain was trying to understand what I said, so I repeated myself."
Witnessing the sudden and grave concern on his daughter and future son-in-law's faces, Grant tried to make sense of what was happening.
"I reasoned that I was probably overheated. I'd also lost my balance, and my future son-in-law was holding me up. I heard my daughter say, 'I think you're having a stroke.’ Next, I remember my wife driving up with our car, and they tried to get me inside. They couldn’t get me easily into the car, so they lowered me to the ground. Then I remember hearing a frantic phone call to 911."
Sudden Concerning Symptoms
Grant resisted the idea that something was very wrong. He simply wanted to go home. His family refused, listing these reasons:
- The left side of his face had gone slack.
- He couldn't stand on his own.
- His speech was unclear.
Straight away, Grant heard sirens. Emergency medical services (EMS) arrived — beginning with a fire truck. The workers lay Grant on the ground and began taking his vitals.
A Daughter as Health Care Advocate
Grant's daughter, a trained medical professional with a doctorate in physical therapy, began advocating for him to receive tissue plasminogen activator (tPA) to dissolve his brain blood clot. She informed the EMS team that she was certain her father had suffered a stroke and that time was of the essence to dispense the drug.
"My daughter was adamant and asked for the drug to be administered."
Grant's wife also quickly chimed in, asking them to take him to whatever nearby hospital was most equipped to treat stroke patients and receive tPA. EMS determined that WakeMed Cary Hospital was the best choice.
"I remember being loaded into the ambulance and, at one point, an EMS worker asked if I was going to be sick since I'd mentioned feeling nauseous."
Hoping to lighten the mood, Grant cracked a joke.
"The EMS worker had introduced himself as TJ (similar to the 80s TV action star). I replied, 'TJ Hooker, please tell me you didn't slide across the hood of the ambulance before getting inside to come get me.'"
They all enjoyed a hardy laugh.
Swift Transport to WakeMed Cary Hospital
Upon arrival to WakeMed Cary Emergency Department, pulmonologist Amarpreet Kaur, MD, admitted the patient and acted as his attending along with hospital medicine attending physicians Qing Chen, MD, and John Langhenry IV, MD, and the care team stepped into action, performing a computed tomography (CT) scan to confirm blood clots in Grant's brain caused an ischemic stroke.
Providers Hughes Burridge, PA, and Wake Emergency Physician Madjimbaye Namde, MD, then connected with the telestroke team, so a neurologist could advise of next steps.
Grant was given Tenecteplase, and the team noted he still exhibited some deficits (mainly around sensation and visual acuity), so Burridge, PA, and Dr. Namde coordinated a transfer to WakeMed Raleigh Campus catheterization lab for a thrombectomy.
“I want to recognize the amazing folks I did not get to meet at the information desks in the Cary Emergency Department and at Raleigh Campus. They made my family feel at ease and helped them understand where I was and where they could wait comfortably and stay informed. Literally, every single person we encountered at WakeMed was so kind and empathetic. We are very grateful.”
Intra-arterial Mechanical Thrombectomy
Neurosurgeon Brandon Burnsed, MD, of Raleigh Neurosurgical Clinic, performed a thrombectomy, removing two clots, aided by the care team, consisting of Matt, Emily and Amanda.
Intra-arterial mechanical thrombectomy is a minimally invasive procedure that, when performed in conjunction with Alteplase administration (similar to tPA), can remove clots and stop a stroke in its tracks. The results can minimize or completely eliminate the long-term side effects of stroke, such as speech, dexterity and mobility issues.
During the thrombectomy procedure, Dr. Burnsed used an innovative, catheter-based technology to capture the clot and pull it out of the artery, which restored blood flow to his brain. This procedure was performed using BiPlane technology, an advanced imaging system that helped Dr. Burnsed guide instruments through Grant's artery to the clot. WakeMed is a Value Partner with Siemens Healthineers, makers of the Artis Icono BiPlane technology used in thrombectomy procedures.
Recalling this experience, Grant jokes, "I remember being on the procedure table and having the sensation of my pants falling. Matt explained to me that he was preparing me for the insertion of the catheter, and in that moment, I knew exactly what he meant as I recognized the sound of the electrical trimmer that they use at the barber shop."
Grant remembers teasing Matt, "'There are sensitive parts down there I don't want cut, so do be careful.' Matt's response was very professional. He explained that he was clearing the area, so they could carefully insert the catheter."
The catheter traveled from Grant's groin up to his brain. Simultaneously, the procedure team played Grant's favorite Star Wars music to soothe him during the semi-awake procedure. Dr. Burnsed and team successfully removed the clots.
Afterward, Dr. Burnsed visited Grant's wife, daughter and future son-in-law in the waiting room. He explained that they expected Grant to make a complete recovery. He also joked this was the first time he'd had a patient talk throughout the entire procedure.
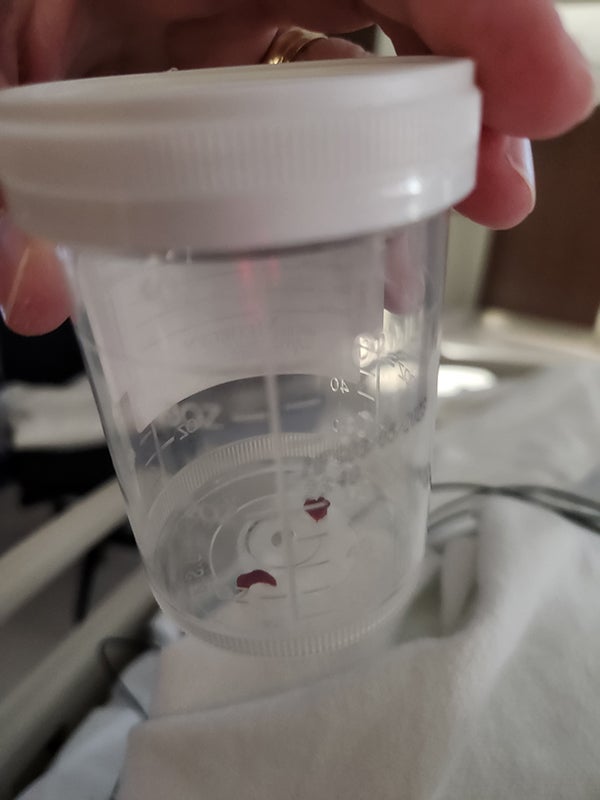
Grant had asked during the procedure if he could keep the clots, and Dr. Burnsed placed them in a vial for Grant to take home.
"I was curious to see them as they were so curiously small yet could have ended my life. I now keep the vial on a shelf at home and when I'm feeling too lazy to exercise or want to indulge in unhealthy foods, I look at it as motivation to make the right choice."
Gratitude for Brain-Saving Care
Realizing the brain-saving care he received on that fateful Sunday, Grant shares, "Dr. Burnsed, Matt, Emily and Amanda were amazing. I was awed that Dr. Burnsed could run a stent remover into my brain and retrieve the clots. It seemed like science fiction. Emily, Matt and Amanda were fantastic in keeping my family informed and putting me at ease. I'm incredibly grateful to Dr. Brandon Burnsed and team for doing the procedure."
Following his procedure, Grant was transported to the Neuro Intensive Care Unit (ICU) under supervision of pulmonologist Trevor Taylor, MD, and hospitalist Divyesh Mehta, MD. Care team members Kimberly, Ashley and Leslie monitored him, offering comprehensive around-the-clock care.

Grant comments, "They made me as comfortable as possible, given the events that had unfolded. They made my family and me feel remarkably at ease. I'm awed by the provision of topnotch care when our whole world was shaken. Kimberly was the first wonderful nurse. Ashley took over in the evening and ensured I got what rest I could, despite all the tests and checks. The following day, Leslie helped me get up to test movement with the physical therapy staff. I got to walk, so she quite literally got me back on my feet."

The Echo Bubble Study
While in the Neuro ICU, Grant received an echo bubble. Care team members Holly and John performed the study, which involved a saline injection that was mixed with Grant's blood to form small bubbles. The purpose was to identify if he had a hole in his heart, formally called a patent foramen ovale. This study helped determine a possible cause of his stroke.
"I'm the curious, talkative type," admits Grant. "I asked numerous questions throughout the study, as I have always heard air in the blood flow is bad, and they patiently explained exactly what they were doing and why, showing me pictures of what they saw. They shared that the doctor would review and share the results a bit later."
Results revealed that Grant's heart was fine and not the cause of his stroke. In the evening hours, Grant was moved to a step-down unit. He and his family received care from kind and informative staff on duty, including Sindra, Luis and Sierra. They conducted routine follow-up tests, seeking signs of another clot or stroke, while also keeping the family informed and assuring them of his remarkable recovery.

Discharge Home and a Return to Normal Life
On late Wednesday afternoon, May 29, Grant was discharged home after the physical, occupational and speech therapy teams determined his balance, sight, fine motor skills and speech had returned.
"I remember having trouble swallowing after arriving at the hospital. I also had some neuropathy in my arms and legs, but by the time I was discharged, my swallowing and feeling sensations had returned to normal. I truly feel it is nothing short of a miracle."
Within weeks of returning home, Grant also noticed his energy level had returned. He'd gone home from the hospital a bit fatigued, but was soon back to mowing the lawn, going for walks and doing other activities around the home. Not long thereafter, he also went back to work in information technology.
'Time is Brain' Made Clear with a Visit to the WakeMed Stroke Support Group
In June, Grant decided to join WakeMed's virtual Stroke Support Group to share with other patients his journey of experiencing a stroke and navigating recovery.
"I was one of the truly fortunate ones who made a complete recovery, so in the group I felt a bit of guilt for my remarkable outcome. Yet, I'm thankful. I think it was divine intervention that my daughter was in town and with me at the moment it happened. She immediately recognized my stroke symptoms and advocated for my life-saving care."

About WakeMed Stroke Program
Each year, thousands of families in our community are impacted by stroke — a brain attack that can occur at any age.
At WakeMed, we offer a full continuum of compassionate, innovative stroke care — from diagnosis in our emergency departments to rehabilitation in both our award-winning inpatient and outpatient facilities.
As leaders in stroke care, we also collaborate with hospitals through our Telestroke Program to ensure that patients in various regions of the state receive the timely support required to recover from stroke.
WakeMed's Award-Winning Stroke Program
WakeMed Raleigh Campus and Cary Hospital are Joint Commission Thrombectomy Capable Stroke Center and Joint Commission-Certified Primary Stroke Center that also performs Thrombectomies. We’ve also received the Joint Commission Gold Seal of Approval for Stroke Care.
Our Stroke Program is distinct in providing a comprehensive approach, moving from prevention to management. Our dedicated team of specialists, renowned for their expertise, use physical medicine and rehabilitative techniques at strategic steps along the route to recovery to support the best outcomes. Here are just a few of our impressive features:
- Collaboration with EMS providers to facilitate rapid assessment and transport to the hospital
- Team approach that helps minimize time from arrival to administration of thrombolytics
- Availability of neuroradiologists for quick, expert interpretation of imaging
- Neurology and neurosurgery coverage 24 hours a day, seven days a week for evaluation and treatment
- Neuro intensive care unit for optimization of care for patients with severe strokes
- Nursing staff skilled in assessment and care of stroke patients
- Designated nursing unit for the care of patients with neurological and neurosurgical diagnoses
- Interdisciplinary care planning involving physicians, nurses, case managers, therapists and other services such as nutritionist consultation and pastoral care
- Comprehensive post-discharge rehabilitation services, including specialty services such as vestibular rehab to treat dizziness and vertigo and stroke VNS rehab to improve upper limb function for stroke survivors
- Public education and awareness programs that focus on risk factor reduction for stroke prevention
- A variety of stroke support groups at several locations throughout North Carolina
WakeMed has also been awarded top honors from the American Heart Association and American Stroke Association for success in implementing a higher standard of care for stroke patients. We are accredited by the Commission of Accreditation on Rehabilitation Facilities (CARF), due to our comprehensive inpatient rehabilitation programs and commitment to specialty rehab. Our Stroke Program is Stroke Specialty Program Certified (CARF-SSP).
Additionally, WakeMed Raleigh Campus has received official certification as a Thrombectomy-Capable Stroke Center from The Joint Commission. This certification is the second highest of the four advanced stroke certifications offered by The Joint Commission in collaboration with the American Heart Association/American Stroke Association. This certification recognizes hospitals that meet rigorous standards for performing endovascular thrombectomy and providing post-procedural care for patients.