Treatments
In this section:
- Thrombolytics (clot busting medication)/Thrombectomy (clot retrieval procedure)
- Angioplasty and Stenting
- Coiling/Clipping/Neurosurgical Care
- Primary and Secondary Prevention
- Stroke Vagus Nerve Stimulation Rehabilitation
- Stroke Quality Metrics
At WakeMed, our Joint Commission-certified Thrombectomy-Capable Center team demonstrates skill and expertise, using the latest tools to reduce the length of stay and mortality in cases of stroke.
Thanks to dramatic advances in technology and the way strokes are treated, more Americans are surviving strokes and experiencing fewer permanent side effects than ever before.
Treatment Options
Once at the hospital, the patient will need to have blood tests as well as a computed tomography (CT) scan to determine if and where a clot exists.
These treatments include:
Ischemic Stroke Care

Thrombolytics (clot busting medication): Tenecteplase
- This medication is offered 24/7 for the emergent treatment of acute ischemic strokes.
- This medication is only used to treat stroke within 4.5 hours of stroke onset. Time is of the essence! Please review stroke symptoms to learn about recognizing stroke and getting to the emergency department as quickly as possible.
Thrombectomy: Procedure to Remove Clots
Intra-arterial mechanical thrombectomy is a minimally invasive procedure that, when performed in conjunction with Tenecteplase administration can remove clots and stop a stroke in its tracks. The results can minimize or completely eliminate the long-term side effects of stroke, such as speech, dexterity and mobility issues.
During the thrombectomy procedure, doctors use an innovative, catheter-based technology to capture the clot and pull it out of the artery, which restores blood flow to the brain. This procedure is performed using BiPlane technology, an advanced imaging system that helps guide instruments through the artery to the clot. WakeMed is a Value Partner with Siemens Healthineers, makers of the Artis Icono BiPlane technology used in thrombectomy procedures.
The procedure is performed 24/7 by neurointerventionalists in the cath labs at WakeMed Raleigh Campus and WakeMed Cary Hospital.
Permissive Hypertension
For patients who are unable to receive the clot busting medication or clot retrieval procedure, neurology providers may recommend allowing their blood pressure to remain elevated to better perfuse the brain for a brief period of time.
Angioplasty & Stenting

Angioplasty, a procedure commonly used to open blocked coronary arteries, is also an option to return blood flow to the brain for some stroke patients.
In this procedure, an interventionist threads a catheter containing a balloon to the site of the blocked carotid artery, and then inflates the balloon to open the artery.
The interventionist may also place a stent, a tiny device made of metal mesh, at the site of the blockage to help prevent future blockages that could cause strokes.
Learn more about WakeMed's vascular surgery options.
Hemorrhagic Stroke Care
Brain Bleed
- Aneurysm coiling/clipping
- Blood pressure control and blood thinner reversal
- These measures are taken immediately upon identification of a brain bleed to attempt prevention of increased bleeding.
- Neurosurgical services
Primary and Secondary Prevention
- Depending on your health history and brain imaging results, you may be prescribed medications to prevent a future stroke. If you are prescribed these medications, it is critical to fill the prescriptions and take them as ordered to reduce your risk of stroke.
- Here are example medications:
- Anticoagulants (blood thinners)
- Antiplatelets
- Antihypertensives (blood pressure medications)
- Statins
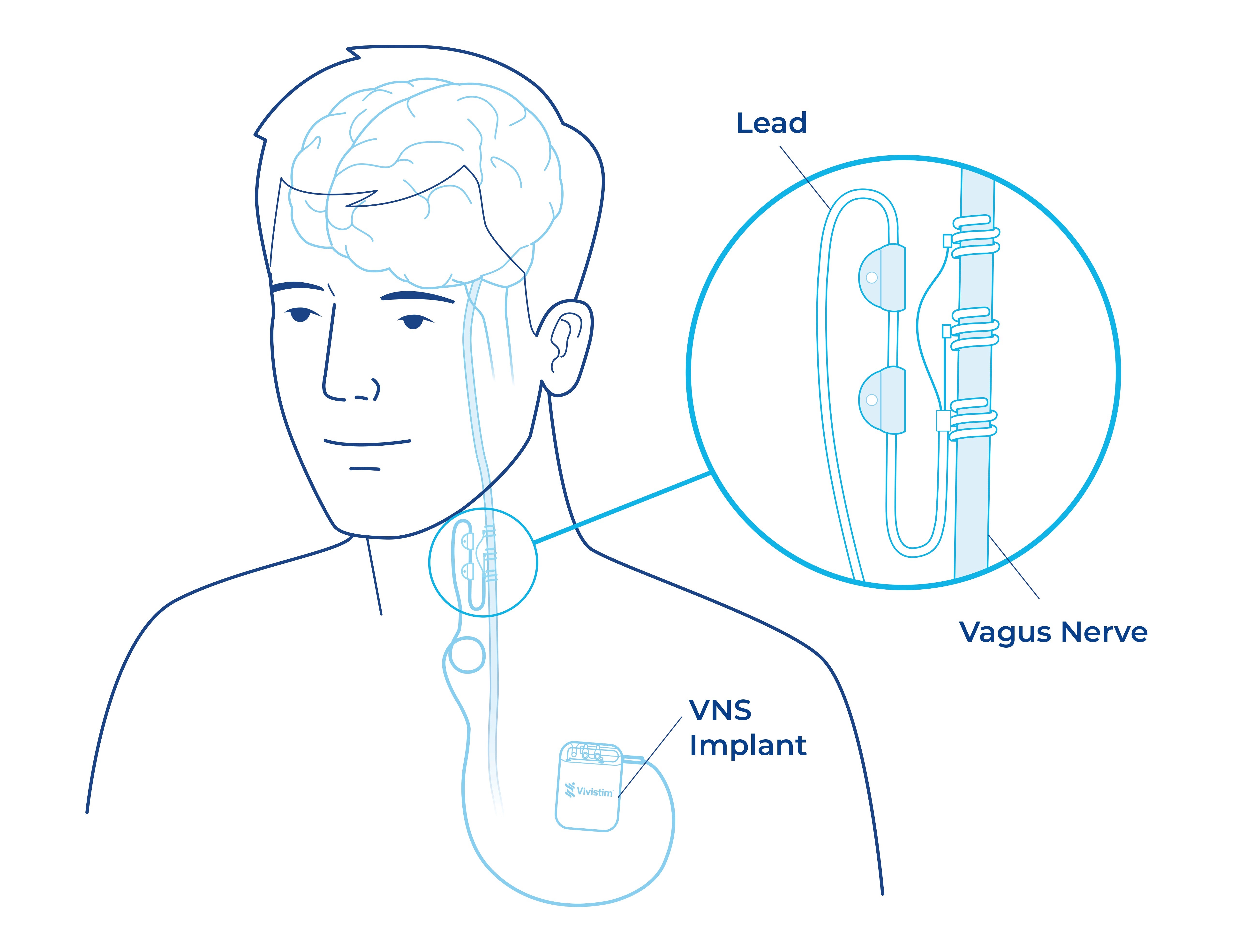
Stroke Vagus Nerve Stimulation (VNS) Rehabilitation
A neurostimulation device that helps stroke survivors regain their independence and improve their quality of life.
After experiencing a stroke, nearly 60 percent of survivors continue to suffer from persistent impaired upper limb function and weakness. This period is often referred to as a recovery plateau, which means their condition stops improving and indicates the problem isn’t in the muscles, but in the brain or the nerves.
Stroke VNS Rehab Can Help Create New Neural Pathways
WakeMed offers a safe and effective breakthrough treatment via a small, implanted FDA-approved device that improves upper limb function for stroke survivors who have not yet regained hand and arm mobility after active rehabilitation therapy, even years later.
Within WakeMed’s Stroke Program, neurosurgeons, neurologists and occupational therapists collaborate to offer vagus nerve stimulation (VNS) during therapy to improve upper limb function for stroke survivors.
When used in combination with outpatient occupational therapy and at-home activities, the VNS stimulation activates the parts of the brain (via the vagus nerve) that are important for motor learning and generates two to three times more hand and arm function for stroke survivors than occupational therapy alone after six weeks of outpatient therapy.
Even if a stroke happened years ago, patients may experience increased hand and arm function over time. When the stroke VNS therapy boosts the brain’s neural activity, it builds lasting connections that continue to work even when the implanted device is not in use.
Benefits of Stroke VNS Rehab
Users report improvement across numerous qualities of life measures, including:
- Increased functional mobility, as early as two to three weeks
- Improved self-care such as preparing meals, getting dressed or playing cards
- Positive daily living
The Process
1. Same-Day, Outpatient Procedure
The device is placed during a short outpatient procedure, typically by a neurosurgeon. The device is placed under the skin of the chest and the lead is tunneled from the neck to the generator.
Similar procedures safely performed for 25+ years to treat other medical conditions.
2. Intense Outpatient Therapy
An occupational therapist uses a button to activate the neurostimulator repeatedly during rehab tasks. Most patients do not feel the stimulation.
3. At-Home Therapy
Patients can activate the device at home during rehab or daily activities using a special magnet.
Is Stroke VNS Rehab Right for You?
Stroke VNS Rehab is intended for chronic ischemic stroke patients with moderate to severe arm and hand impairment six months after stroke. If you think you may benefit from Stroke VNS Rehab, speak to your health care provider about receiving an evaluation with a WakeMed rehabilitation professional to see if you are an eligible candidate.
If you pass the initial rehab assessment, you will then be referred for a consultation with a neurosurgeon to determine if you are a good candidate for the implantation procedure.
For more information about Stroke VNS Rehab, call 919-350-7000.
Stroke Quality Metrics
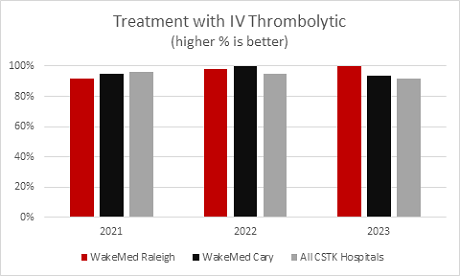
This chart shows the percentage of patients that arrive within two hours of their “last known well” and receive the clot busting medication within three hours of their last known well. The “Last Known Well” is a critical timeframe that the care team uses to determine stroke onset and treatment eligibility, as the clot busting medication can only be used within 4.5 hours of stroke onset.
In 2023, 82% of ischemic stroke patients who arrived to the hospital within 4.5 hours of stroke symptom onset and received Tenecteplase were able to discharge home or to acute rehab.
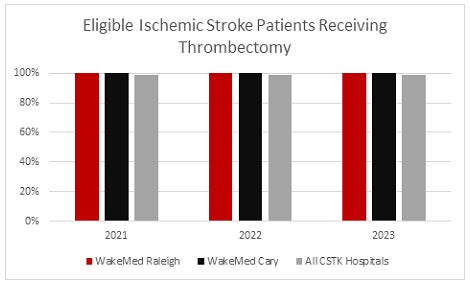
This chart shows the percentage of ischemic stroke patients who meet criteria for clot retrieval or thrombectomy and are accepted for the procedure at WakeMed. WakeMed consistently meets 100 percent for this metric, indicating that our care teams are keyed in to recognizing signs of a large ischemic stroke, identifying criteria for this procedure and getting patients to the neurointerventionalist and Cath Lab team!
Telestroke
In addition to these treatments, WakeMed offers an innovative Telestroke program to support stroke patients at hospitals with less medical access, thereby making them stroke capable. The program is a form of telemedicine, providing patients with enhanced in-house stroke care and 24-hour access to stroke neurologists.
Using Telestroke system carts and a two-way live video, audio and image sharing system, consulting stroke neurologists can evaluate a remote patient in real time to diagnose a stroke and determine the best course of action. Patients also receive streamlined access to WakeMed for advanced and post-stroke care.
If you think you or someone you’re with is having a stroke, call 911 and get to your closest emergency department. The faster the treatment, the better the chances for a full recovery and return to normal life.
